Alcohol can prove to be detrimental in more ways than one, but the liver is where its hammer stroke will fall the hardest. Alcohol-related liver disease (ARLD) refers to liver damage that happens because of drinking heavily over a period of time. It can lead to inflammation, scarring, and other complications like the build-up of fats, bleeding, and even liver failure. In extreme cases, ARLD can require a liver transplant to prolong the survival rate and prevent fatality.
Early Signs of Alcoholic Liver Disease
As we mentioned before, ARLD is often not detected until it is too late. So, when you understand the early signs of the disease, you can seek early intervention and reverse this condition:
- A general feeling of being ill
- Abdominal pain
- Vomiting
- Diarrhea
- Decreased appetite
If you or a loved one is consuming alcohol and experiencing these symptoms, then it can be an indication that the drinking has started to impact the liver. Seeking early intervention and treating AUD can stop this condition from worsening further and even reverse it. But if the drinking continues, then it leads to a quicker progression of the disease to the point that it becomes irreversible.
Find Help for Alcohol Addiction and ARLD at Design for Recovery
Alcohol-related liver disease is not only damaging to the liver, but as the condition worsens, it can even reduce life expectancy rates as well. Therefore, controlling alcohol consumption is vital to managing this condition.
When you make the decision to recover from alcohol use disorder, you are making a very empowering decision that will positively affect your entire well-being and life. While it is challenging to quit alcohol on your own, with integrated care options, a sober life is closer than you think. Design For Recovery provides premier sober living homes for young men, defined by a structured environment, peer accountability, and a sober future ahead of you.
- What Is Alcohol-Related Liver Disease (ARLD)?
- Stages and Types of Alcohol-Related Liver Disease
- Early Signs of Alcoholic Liver Disease
- Advanced Symptoms of Alcohol-Related Liver Damage
- Treatment Options for Alcohol-Related Liver Disease
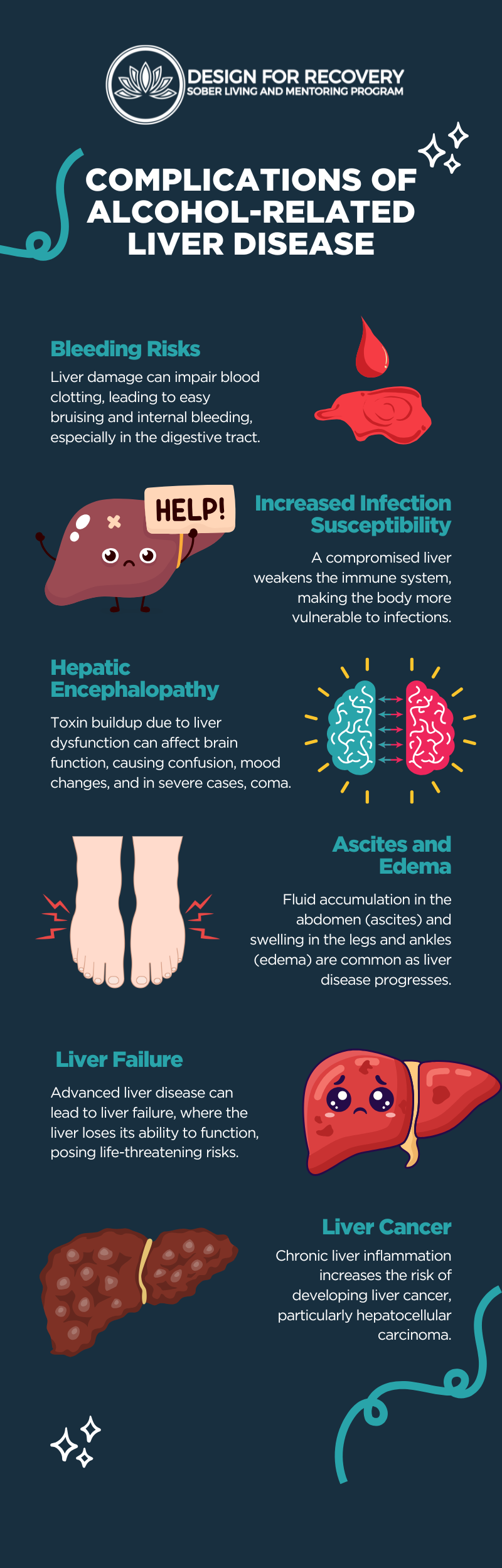
- Complications of Alcohol-Related Liver Disease
- How to Prevent Alcohol-Related Liver Disease?
- Find Help for Alcohol Addiction and ARLD at Design for Recovery
Begin Lasting Sobriety Now!
Frequently Asked Questions
ARLD refers to liver damage caused by heavy and prolonged alcohol consumption.
Common early signs of ARLD are fatigue, abdominal discomfort, and unexplained weight loss.
Yes, in the early stages of ARLD, it can be reversed by abstaining from alcohol use. However, once it progresses to the cirrhosis stage, it becomes irreversible, and one may even need a liver transplant.
Treatment for ARLD includes medications, lifestyle modifications, psychotherapy, nutritional therapy, and, in severe cases, a liver transplant.
Avoiding or moderating alcohol intake while also maintaining a healthy lifestyle is key to preventing ARLD.
https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/understanding-alcohol-use-disorder
https://www.ncbi.nlm.nih.gov/books/NBK436003/
https://www.ncbi.nlm.nih.gov/books/NBK546632/
https://www.hopkinsmedicine.org/health/conditions-and-diseases/alcoholinduced-liver-disease
https://www.cdc.gov/nchs/fastats/alcohol.htm






Written By
David Beasley